Tick. The final infusion of the three 21-day cycles of chemo is done. I’ve been of a mind to follow Alan Bennett’s excellent observation that he doesn’t wish to be so familiar with the treatment as to call it by its nickname. But adding the ‘therapy’ each time has become peculiarly tedious and needlessly pointed. Back when, I used to pronounce R.D. Laing’s name the way it’s spelled, as he did. But everyone asked who I meant and then corrected me, ‘Oh, you mean Lang,’ so I gave up and called him Lang with a twang like everyone else for the simpler if less self-righteous life. So chemo’s over.
A week after the last infusion, I was scanned from head to abdomen to see what, if anything, had happened. Just once the technician said ‘brain’ instead of ‘head’ and my careful poise unravelled, though not so far that it could be seen from the safety of her glass box. Maybe that brain-frazzled moment will show up on the scan as a bright spike in the terror region of my brain. The amygdala? The little almond, like the rusks called mandelbrot with their embedded almonds which I went on my child’s scooter every Sunday to buy from Grodzinski’s in Goodge Street. Next week, I see the Onc Doc and get the result of the scan, and the go-ahead or otherwise, for a month of daily radiotherapy at Addenbrooke’s. Weekends off, just like a regular job.
So now I’m dawdling in one of those grossly extended weeks that one endures while waiting for lovers to phone or scans to be assessed. Why don’t the lovers ring, and the doctors assess, the next day? Because: be reasonable. You’re not the only fish; not the only one with cancer. The world has its timetables and rhythms. It was precisely for weeks like this that our parents were supposed to have taught us to put aside childish notions of instant gratification for the more mature deferred sort. As we all know, come cancer scans and silent lovers, it doesn’t work. So I’m living with Schrödinger’s tumour. There it is: both smaller and bigger; spreading via the lymph nodes to the brain (or whoknowswhere) and halted in its tracks; in receipt of the good fortune (20-30 per cent) of a remission of unknown length, and the bad luck (70-80 per cent) of no remission. Until Onc Doc opens the box next week. I am interested in his opening gambit. The diagnosis came with ‘What were you expecting from this appointment?’ I imagine the opener to the scan results will be more of the ‘Which do you want first? The good news or the bad news?’ kind, because I’m beginning to get the idea that there aren’t going to be any ‘it’s this or that’ statements any longer. Superposition right up to the end, both more and less until the final opening of the final box, the upshot everyone faces, some having had more warning than others, sooner rather than later or later rather than sooner. Very few of us have an actual date even to pencil into our diaries, ‘and so,’ as Malone says, ‘grow gently old down all the unchanging days, and die one day like any other day, only shorter’.
And what of the chemo? Some of the things everyone knows and dreads. Not all. Insane tiredness and chemo-brain, the latter not a Z-list superhero but an ugly fact of life as acuity and the capacity to hold anything in the mind for more than a moment drains away. ‘You told me that, when? You did not. I’m the person round here who remembers everything. Remember? You did not tell me.’ But when I had to ask the other day about a plot point in Law and Order, I knew it was my game that was up. Chemo-brain and tiredness like I’ve never … In spite of which I’ve tried to think myself into a state of meerkat alertness, to be, in this part of the memoir at least, a proper hack, close enough to the other side of treatment to report my findings on practical day-to-day living with an inoperable cancer diagnosis and the treatment for it. Answer: there is no practical day-to-day living with chemo and a certain uncertain prognosis. I gather that some people have chemo and go to work every day, undaunted. I am one of the daunted. The final infusion of poison last week came with an additional two units of someone else’s blood to improve my low and unregenerated white blood cell count, and fix the anaemia that showed up in the blood tests they do so regularly. Iatrogenic disorders, but at least we know that the poison in there is killing something, the good along – it’s to be hoped – with the bad and the ugly. So I spent seven hours – usually it’s a couple of hours – attached to the cannula attached to a tube leading to bags of liquid hooked to the top of the chrome stand with a machine in its middle to regulate the drip, drip, drip.
Chemo-brain doesn’t just dim my lights, it also has made me feel clumsy, not completely in control of my movements, as if the regular puppeteer is no longer the only one pulling the strings attached to my hands and feet. My superfast typing has many more errors, and I’m very wary of going down stairs or reaching for a glass. The main preoccupation, however, of the seven-hour infusion was knowing there was no way to avoid my drip-buddy and me going abroad for a trip to the loo. It looks easy on the telly, when the cancer patients roll their drip stands along beside them as if they’re taking them for a stroll, one arm outstretched to enclose the upright like an arm around an old friend’s waist. It felt more problematic than that to me. Planning was required: any dancer will tell you that you should ‘walk’ through a movement in your mind, as well as stepping it out on the floor. I had to try to disregard the image of my contraption and me flat out, me hapless, the machine broken, and both of us dribbling pools of blood or escaped carboplatin (platinum, my precious toxin) from my cannula and its disconnected connecting tube. Think it through, instead: get down from the high-off-the-ground, blue airplane chair; negotiate the bump at the threshold of the bathroom; manoeuvre it and me sidlingly in order to get the door shut.
Because I knew I would have to, there was hardly a moment of the seven hours when I didn’t think about needing a pee, but I managed to restrict it in actuality to just the once. The occasions when as an adult I’ve had to give so much consideration to urinating have been few; most memorable was in the Swedish Arctic at 40 degrees below freezing, failing to sleep in a tent pitched in a field containing seven thousand reindeer. I spent most of the night visualising the enormous difficulty of getting out of my sleeping bag, managing not to step on any of the four other people and one dog on my way out of the tent, struggling with the several layers of all-in-one and upper and lower clothing designed to make the peeing process a zip for men, but requiring me, without a distance-spraying organ, to expose practically all of myself to the herd of untroubled reindeer, while I murmured strong curses for their ears only, and my pee and lower body froze in the crazily cold starry night. Eventually I just had to do it. It was neither dignified nor comfortable. But it was at least quite exciting and the sky certainly the starriest I’d ever seen. For the 63 days of chemo, even when not attached to a drip pole, my life has been largely made up of similarly lengthy considerations of mundane domestic and personal matters – get up, wash, dress, work, read a book, make a cup of tea, make a hot-water bottle, watch TV – and whether I can give a fuck about doing all, some or any of these things, or not-giving-a-fuck-withstanding, and going against every cell of my state of being, I should or could make the effort. The answer is, with the exception of the overwhelmingly desirable hot-water bottle, invariably no.
I was warned in advance about the cancer-and-chemo tiredness, the aetiology in both cases still essentially a mystery to medics, but for most people unavoidable. This I knew. I’d read diaries and seen TV and movies that dealt with this most feared and undesirable intervention. There is no treatment for the tiredness, as there is for the nausea, the other notorious side-effect that overtakes you. After a bad few days with nausea in the previous cycle, for the final infusion I took home four different kinds of anti-emetic, fine-tuned to take account of my earlier reactions. I don’t even have to suffer the universal (I thought) mark of the canceree, her badge of baldness, because for some reason this kind or quantity or something of chemo had no interest in killing off my hair follicles. So I am grateful that chemo for me was not as devastating and disfiguring as it might have been; neither bald nor bescarfed, or throwing up, and thus signalling to friends and strangers which world I’m currently inhabiting, causing them in the other real world to shout across their sympathy and helplessness at me or scurry by in embarrassment. To strangers at least I’m just a regular stranger. That’s something, or it would be if I went out anywhere apart from the oncology unit.
I listened to the Onc Doc’s warning about tiredness at the original appointment, and wondered if he could imagine the extent to which I have always been indolent and agreeably attached to my sofa or bed. ‘I have the metabolism of a sloth,’ I explained. He said: ‘This is different.’ I thought: he thinks I’m exaggerating. Everyone thinks I’m exaggerating because they can’t imagine contentedly spending a week or two – or three – not leaving the house, not once, and then finding it an insufferable intrusion to have to attend an appointment or even answer the phone. It’s not a malaise, or if it is, it’s my malaise and a condition I treasure. It’s not a phobia, it’s a choice. The Onc Doc and Onc Nurses talk about ‘fatigue’, not ‘tiredness’, as if to distinguish it in kind from feeling sleepy or lazy, just as major depression is distinct from ‘a bit mis’, or dehydrated is many steps along from thirsty or always carrying around a non-prescription bottle of water and taking a few sips from time to time. Fatigue isn’t more tired than tiredness, it’s differently tired. You can’t feel the carboplatin as it travels through your veins, but you can feel fatigue in them later, as though they were filled with sluggish liquidised metal (mercury, say, but without the ‘quick’ of quicksilver) dragging its weighty way around your body, to your arms, legs, head, fingers, torso, and to eyelids that feel so heavy they threaten to drain down into a viscous puddle at your feet, your veins imploded and sucked dry by a monstrous gravity. Anyway, very tired. Fatigue.
A regular day now might unfold with me doing some work in bed and then getting up. Showering or bathing and dressing, and then, all clean and ready for the day, the body and mind refold themselves, suddenly faced with the urgent decision whether to eat something or to get back into bed straight away, not stopping for food, to sleep for four more hours or so. With or without breakfast, the effort of getting up finishes the day off for me. I’ve tried it the other way round, getting up first, before work, but then that’s as far as I get, so no breakfast and no work, just peeling off the clothes I’ve just put on and creeping back to bed, with nothing done, but mightily relieved to have been let off the exhausting business of making a decision. Logically, I should stay in bed all day and work intermittently, like snacking, as well as snacking intermittently like snacking. But my brain and muscles turn off after a while of working, so I’d have to go back to sleep again, anyway, not dozing, no forty winks, but deeply, fast, vastly asleep. And as the Macmillan Nurse booklets (every patient’s and, it seems, every doctor’s source of information) explain, this fatigue is not alleviated by rest. You wake up just as exhausted as you were when you went to sleep. In an aside, they say that the fatigue can last between two months and two years after the chemo has finished. In a few months (or years) of days like that, a full consideration of the necessity or otherwise of having a pee counts as quite exciting enough. I’ve tried but failed to watch a full-length episode of Lovejoy, the Poet’s favourite after a day wording and teaching, but my lowered excitement threshold can’t take the plot tensions or the anguish of seeing those familiar youthful faces of now-aged English actors who you just can’t put a name to, though it’s on the tip of your tongue. That’s how fatigued I’ve been. After the blood transfusion, I’d hoped for something like Popeye’s transfiguration after downing a tin of spinach, but I was still pretty tired in the days after. I could sleep in a heartbeat, but my veins were filled with something lighter than mercury, and my body was not so determined to join in with my mind’s unchanged exhaustion. It was an improvement, but by Day 6 the full weight of exhaustion – had the new blood run out? – hit me like a wrecking ball and I spent that weekend asleep for ten and more hours of daytime after eight or nine hours at night.
Days, by the way, are my new way of telling time. They are the units of chemo, Day 1 to Day 21, after which it all starts again at Day 1. Day 6 or 7 is the lowest ebb and in each cycle I have to start a course of antibiotics to fend off infection. I’m supposed to pick up by Day 15 or 16, my blood recovering, but I’ve never noticed it, and the need for the blood transfusion last time suggests that my body isn’t playing strictly to the prescribed rhythm. The body, we shouldn’t be surprised to learn, has a mind of its own.
The chemo period, for all the deadness of feeling and lack of fine-tuning, threw a lasso round my life. Until the three cycles were complete nothing else was going to happen. There was stasis in the other, non-cancer life. Not just exhaustion, but a lack of will even to investigate what was going on inside me. I feel I’ve allowed myself more ignorance about the nature and behaviour of my cancer than I’d allow myself if I had the flu. I am not a doctor, but there’s the internet and I’m still capable of reading, if not retaining, say, a juicy paper at Academia.edu: ‘Things Fall Apart: Heidegger on the Constancy and Finality of Death’ (by Taylor Carman), so how come I’ve remained so foggy about the details and possible trajectories of my cancer? I tell myself it’s because I’m not so much in charge in cancer-world. I don’t think I’ve ever felt so not in charge. This is one of the surprises of being cancered. I don’t approve, but I don’t have the energy to roll up my sleeves and find out everything there is to be found. The exhaustion makes me incapable, but there is also some absence of will to find everything out. On the other hand, it’s also increasingly clear to me that there may be little to find out and that no one, Onc Doc, Onc Nurse, really knows very much, except in an academic way. Everything is presented to me statistically, as probabilities. I can’t find the right question to break through that, to talk about the cancer that is me and mine, what it is, how it is, how it and I are with each other. Something that pans in on the singularity of the particular cancer I’m hosting. I guess it’s because ‘they don’t know’, like they don’t know exactly how or why antidepressants work, but that they do, statistically well enough.
I think, all they can do with me and my cancer is to follow the cancer’s lead. The scan will show if the tumour has shrunk or stayed still, it will show where it has travelled to, ‘except’, Onc Doc explains, ‘where it’s too small for us to see’. This crucial exception means waiting for it to grow (get worse) to know where and how far it has gone, when it will also have moved on to be invisibly small somewhere else. The Red Queen explains it in Looking Glass world: ‘Now here, you see, it takes all the running you can do, to keep in the same place.’ Looking Glass world is more stressful in this respect than Wonderland, my preferred state of being, where participants in the Caucus-race start to run when they like and leave off when they like and ‘everybody has won, and all must have prizes.’ In moments of crisis the Alice books have always offered me the common sense of my situation. They are whispering in my ear incessantly in my cancer life.
The treatment seems to be not so very different from what it was decades ago. A plug-ugly poison that kills off cancer cells faster than it kills off other cells. They think. Then checking to see if it has done anything useful. Maybe it has, maybe it hasn’t. Everyone is waiting to see what is going to happen in order to know what is going to happen. The cancer’s in charge and leading them all a merry dance. Perhaps that’s why I’ve so little taste for investigation. There’s an awful lot of uncertainty for patients and doctors in this cancer business. And uncertainty is what I am least good at. I’ve always been prepared to use extreme measures, find drastic solutions, to put an end to uncertainty in my life. (We are back at my failed training in deferred gratification.) As far as I can see this cancer thing has left me without any measures to use or solutions to find. My sense of being a patient, with all its unwelcome connotations, is inescapable. I might refuse treatment, to which, already, Onc Doc has nodded and said that, yes, that is one path open to me which he would respect. So dumb refusal, too, is incorporated into this world. There is no way to be an impatient, or a mispatient, or even an unruly patient. Cancer-world is so structured that one has to proceed as if one were a grown-up, with all its unwelcome connotations.
What has most surprised me is that as soon as I arrived at the oncology day ward for the final infusion, I found myself anxious, distressed even, that there would be no more visits to the ward. I worried that ‘my’ designated nurse, L., would no longer be available to be called, as she insists, with ‘any little problem, no matter how small’. The kindness of nurses is remarkable. The mystery is not that some are said to be heartless, to have had their fill of sick, moaning patients and claptrap bureaucracy, but that so few are like that. Your anonymity to them – you’re not their pal or their sister – makes their patience and friendliness all the more astonishing and truly valuable if you are sick or frightened. So, hampered as I am at rebellion, I’ve now discovered myself to be a little attached to Nurse L.’s unfailing availability and good humour. In fact I was already, in advance, missing the whole thing: the trips to the ward itself; the reception, and G., the always smiling, carefully dressed receptionist; Schindler’s lift, the world’s slowest elevator, with life-saving equipment on the wall in case it failed to get you there in time; the ghastly brown autumnal prints on the corridor walls hinting too readily at ‘September Song’ (‘the days dwindle down to a precious few’); and even, in a distant way, the other patients. We hardly spoke to one another, but only nodded our heads, because people in various stages of cancer treatment aren’t a group anyone wants to be a part of. My former mother-in-law went to the Bristol centre for alternative cancer therapy and in between juicing fields-worth of carrots, complained until her own death about the letters she regularly received from spouses, informing her that one of their group had died. She said it wasn’t encouraging.
The oncology day ward exists solely for people who are anxious and sick, and their frightened relatives, and is staffed by people trained to deal with those conditions. You might think, I did think, it would be a relief to shake the carpet static from my shoes. Yet, on my last day, I discovered that there was something about the entire, dreaded, much mythologised and allegorised cancer ward and its inhabitants, perhaps the pathos, that attaches you to it, however delicate or elastic the connecting fibre. It took me a few minutes to recognise what I was feeling. Over a couple of months of, as I thought, carefully observed treatment, I’d already become mildly institutionalised. Even while I sat there being infused, I felt the loss of the unlovely place and the nurses who, however kind they might be, you rationally hoped you wouldn’t be seeing again soon. So much for my cold eye on life, on death. I have the feeling of being sent away from a place of safety. Left outside. Peter Pan – Peter Panic: not just the awfully big adventure, also the tap tap tapping on the window to be let back in. And I’m further along the programme, a step nearer the end. Where are the place and people I can turn to now – the ‘designated’ nurse I can call my own? Will there be a person there for me if and when I start the radiation therapy, or will I just go to the room where the machine is housed (its technicians sit in another room to avoid the rays) and be zapped day by day for a month, then wait for another scan, another assessment from the Onc Doc, without having someone on the end of a telephone for ‘any little problem, no matter how small’? What am I, ten years old? At best, I think, at the moment.
That institutionalisation and the inner seethings of loss, I remember well enough from leaving schools both as a pupil and as a teacher, and my stays, long ago, in psychiatric units; the tug, the claim, that such places and the people in them have on your emotions, the falling away of the safety net and the fearful feeling of privation when your time as part of a system runs out. In Hove, during my first hospitalisation at 15, in the small unit where they kept a kindly eye on me, both staff and patients, I’d felt such resistance and fear the day I left with my mother to go and live with Doris. I had three or four particular friends, all strikingly different from one another and from me, but closely woven together as inmates. They expressed real pleasure at my ‘fairy-tale ending’, no resentment that it wasn’t them being taken away to some glamorous London life and being wanted, sight unseen, by somebody. Anyway, one of them said, ‘if it can happen to you it can happen to us,’ so with the generosity of inmates, they allowed me to represent possibility for them. Leaving them was a wrench. Leaving them behind filled me with a sense of unfairness, which, not much later, when I was reading accounts of the Holocaust, I recognised as a minor form of survivor guilt.
They wrote to me in London and gave me the gossip, which was normal for life in the Lady Chichester, but hilarious, wilder and more poignant than most everyday goings-on. Pam, after sitting in a cold bath to shrink her Levis in the approved way, had a panic attack, and had to be cut out of her saturated skintight jeans; Sally hadn’t left her bed for a week and Dr Watt was threatening her with the one-way ticket to Haywards Heath, the big asylum that everyone knew no one returned from; Stuart had done a drawing of a sporran in art therapy, claiming his Scottish origins, he said, but his psychiatrist had shaken his head and looked intently at him. ‘A sporran, you say, a sporran? And what is behind a sporran?’ Stuart, who was famously excruciated at the thought of anything physical, said, ‘A kilt,’ but his shrink wasn’t having it. ‘And what is behind the kilt, Stuart?’ Stuart finally fessed up to owning a penis and had to be put on stronger tranquilisers for a few days. This last story was told in great confidence to Margaret, who said that she didn’t think the confidentiality applied to me as I was no longer part of daily life at the Lady C. Everyone sent their love and, although none of them was a reader or had heard of her, they were eager to know how I, the wannabe writer who had escaped the bin, was getting on in the house of the famous novelist.
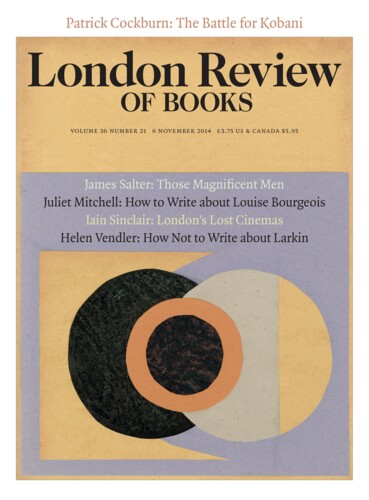
You can read the next instalment of Jenny Diski's memoir here (and the first one here).
Send Letters To:
The Editor
London Review of Books,
28 Little Russell Street
London, WC1A 2HN
letters@lrb.co.uk
Please include name, address, and a telephone number.