Diarrhoea diminishes dignity. In the Western world most people don’t bother to seek medical advice for it, because they are embarrassed and because they expect it to go away soon. They are often right: most community-acquired intestinal infections are self-limiting and get better more quickly if left untreated. This is true even for E. coli O157. Taking antibiotics or antispasmodics is thought to increase the risk of developing the complications of kidney failure, brain damage and cardiac death. But Clostridium difficile is different. Treatment with special antibiotics often works well, but about 7 per cent still die. E. coli O157 outbreaks have much lower mortality rates and infections caused by it are much rarer. In England and Wales in 2005 there were 950 laboratory-confirmed cases; in that year Clostridium difficile caused 51,690 cases of disease and was mentioned on 3807 death certificates.
Clostridium difficile was first described in a 1935 American paediatric journal as a harmless inhabitant of the intestines of infants. The bacterial genus Clostridium has three important hallmarks: a dislike of oxygen, the ability of its free-living form to transform itself into tough heat-resistant spores when environmentally challenged, and the production of powerful toxins. C. botulinum causes botulism, C. tetani tetanus and C. perfringens gas gangrene. The ability of C. difficile to cause a toxin-mediated disease was first recognised in 1978. Its toxins damage the colon; disease manifestations range from mild symptoms to lethal tissue destruction, a spectrum of symptoms known as Clostridium difficile-associated disease, CDAD.
Three circumstances enormously increase the likelihood of developing CDAD: being older than 65, having had previous treatment with antibiotics and being admitted to hospital. Why 30 per cent of infants can have C. difficile in their intestines without falling ill, and why in contrast the old are so susceptible even though a significantly lower proportion of them carry it, is not understood. Antibiotics are thought to kill off friendly intestinal bacteria that compete with and normally suppress the growth of C. difficile. Clearly, many hospital patients are over 65 and many have been treated with antibiotics. But most catch their infections after admission. The bacterium is transmitted by the faecal-oral route; dirty hands are the principal vector. In other words, patients are infected by eating diarrhoea passed by fellow patients. This is the scandal that the Healthcare Commission investigated at Stoke Mandeville and Maidstone.
The scale of the outbreaks in these hospitals was enormous in historical as well as absolute terms. There is quite a rich literature describing outbreaks of infection with root causes of an iatrogenic or nosocomial nature. But few previous disasters match Stoke Mandeville (at least 16 deaths in its first outbreak in 2003-4 and 17 in the second in 2004-5) and Maidstone (about 60 in its two outbreaks in 2005-6). The Lübeck disaster of 1930 (72 deaths from tuberculosis caused by contaminated BCG vaccine) and the 1955 Cutter incident (260 cases of poliomyelitis due to improperly inactivated vaccine, with ten deaths) fall short. Even the enormous Stanley Royd Hospital outbreak of salmonella food poisoning in 1984, with 461 cases and 19 deaths, involved fewer cases: more than 500 became ill at Maidstone and 334 at Stoke Mandeville.
The Department of Health issued guidance documents on the prevention of CDAD in 1994 and 2006, as well as a more general document, Winning Ways: Working Together to Reduce Healthcare-Associated Infection in England, in 2003. But the number of laboratory-confirmed cases of CDAD steadily increased. In England and Wales it rose by 17.2 per cent from 2004 to 2005. Part of the rise is down to a mandatory reporting scheme for cases in patients aged over 65, which was introduced in 2004, and extended to cases in those aged two and over this year. And the number of those at high risk is large, and is rising. For example, in 2005 nearly ten thousand people had operations to repair a broken hip; their median age was 84. But the Healthcare Commission’s investigations do not reveal a picture of hospital managers struggling to do their best against a difficult microbial challenge and seeking guidance from the centre. Rather, at both hospitals they were ‘preoccupied with finances’, ‘had a demanding agenda for reconfiguration’ (both had undergone difficult mergers) and were embroiled in the private finance initiative (PFI).
The impact of financial pressures was to reduce further already low numbers of nurses … there was unrelenting pressure to reduce the number of beds … both trusts … had to open ‘escalation’ beds, often at short notice and in unsuitable environments, without proper support services … The effect of all this was to compromise seriously the control of infection and the quality of clinical care.
Escalation areas were needed to accommodate patients who had to be transferred so that the hospitals could meet national targets requiring that patients spend no longer than four hours in A&E. But an even more effective way of spreading infection was the custom of moving patients from ward to ward. At Maidstone, 50 per cent of medical patients were moved at least once; one patient with C. difficile was moved six times. At Stoke Mandeville, patients with diarrhoea were moved from cubicles and side rooms into open wards to prevent a breach of the A&E target. One physician described ‘safari’ rounds: there were constantly 20 more inpatients than could be accommodated in medical beds, and so patients had to be hunted for on many different wards. Both hospitals had poor quality buildings with too few single rooms for isolating infectious patients; hygiene facilities were inadequate (too few hand basins, for example); control of infection procedures by nurses was deficient.
Many patients suffered and died unnecessarily because of these shortcomings. The Healthcare Commission apportioned a lot of the blame to senior management. The chief executive at Maidstone was difficult to challenge; the trust exaggerated its successes and minimised its problems. It gave inaccurate information to the public. It said that its second outbreak was caused by admitting infected patients from the community. This was not true. It said that it had responded positively to a letter from the chief medical officer about restricting antibiotic use to prevent CDAD when it had not. In public statements it under-reported the number of deaths. Spinning and deception are bad enough. But far worse for the patients were the arrangements for infection control. The director of infection prevention and control was also the director of nursing and patient services. He had no specialist knowledge about infection and spent most of his time on other duties. Infection-control policies were out of date and not properly implemented. The senior infection-control nurse went on sick leave in the summer of 2005, returned for a week in September and retired in October. Her replacement didn’t start work until February 2006. So perhaps it isn’t surprising that a doubling of the already high rate of infection with C. difficile in the autumn of 2005 went undetected and that the subsequent outbreak affecting 150 patients wasn’t noticed.
Arrangements were much better at Stoke Mandeville. The two outbreaks were detected in good time. The infection-control team sent bacterial isolates to the UK reference laboratory, which identified the outbreak strain as a new type, 027, known to be causing problems in Canada. Antibiotic control policies were put in place. But the team’s other recommendations were not heeded. Areas dedicated to infected patients were not provided. The infection-control team submitted a report citing this as of key importance: the document never reached the non-executive members of the trust board. And in order to meet the A&E target the C. difficile isolation ward was closed, against the advice of the team, while the second outbreak was still going on.
The two cases have a much wider significance. The UK ranks poorly among rich countries with regard to the incidence of hospital-acquired infections. It is not a problem confined to a few hospitals. And the shortcomings that led to the outbreaks were not specific to healthcare. They have spelled disaster for other organisations as well, as Diane Vaughan’s analysis of the flaws at Nasa that caused the Columbia and Challenger space-shuttle disasters shows. Nasa had ‘conflicting goals of cost, schedule and safety … Safety lost out.’ Its ‘culture of bureaucratic accountability emphasised chain of command … allegiance to hierarchy and procedure had replaced deference to Nasa engineers’ technical expertise’. Nasa’s structure ‘changed as roles and responsibilities were transferred to contractors’, and its ‘safety system lacked the resources, independence, personnel and authority to successfully apply alternate perspectives to developing problems. Overlapping roles and responsibilities across multiple safety offices also undermined the possibility of a reliable system of checks and balances.’ All these flaws existed at Maidstone and Stoke Mandeville. Vaughan also warned that when changes in organisational structure ‘are put in place, the risk of error initially increases, as old ways of doing things compete with new. Institutional memory is lost.’ Structural changes in the NHS have certainly had this effect. Strategic Health Authorities were created in 2002 and the Health Protection Agency (with important microbiological and epidemiological functions) in 2003. It had local health protection units to which consultants in communicable disease control were transferred from primary care trusts. Each of these bodies thought that one of the others had the lead role in monitoring outbreaks and helping to control them. It is no wonder that the job was done so badly.
The chief executives and board chairmen at Maidstone and Stoke Mandeville are no longer in post. Vaughan writes that ‘changing personnel … has great symbolic value.’ It ‘points to individuals as the cause and removing them gives the false impression that the problems have been solved, leaving unresolved organisational system problems’. She is right. There is no evidence that the status of microbiologists in hospital hierarchies has changed; budgetary pressures on laboratories continue, and the provision of adequate isolation facilities in hospitals remains only an aspiration. And the microbes are evolving in real time.
In May 1900 the ‘Report of Drs Mott and Durham on Colitis or Asylum Dysentery’ was presented to the Asylums Committee of the London County Council. Among other things, Mott and Durham recommended that accommodation provided for isolation should not be used for other purposes, that patients with a suspicious diarrhoea should be isolated, that all cases of diarrhoea should be notified, that ‘while recognising the desirability and necessity of the transference of patients from ward to ward for purposes of treatment and administration, great discretion is necessary when diarrhoea, however slight, exists,’ and that much attention be paid to staff training, disinfection and handwashing. London asylums were publicly funded, and were in that sense precursors of the NHS. Clearly, institutions forget. Like Mott and Durham’s, the Commission’s reports pull no punches. Colour photographs illustrate beds jammed together and commodes contaminated with faeces. These reports bear comparison with the work of the mid-19th-century lunacy commissioners, in particular Samuel Gaskell (brother-in-law of Elizabeth). When he inspected, institutional food was eaten, privies visited, and every patient interviewed.
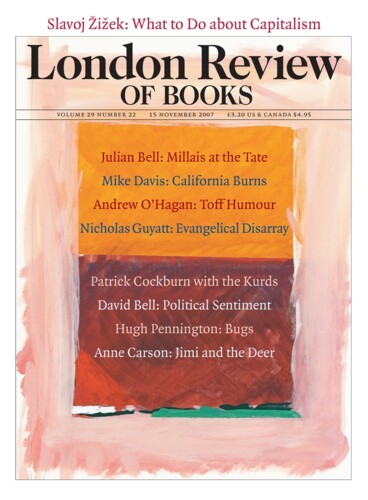
Send Letters To:
The Editor
London Review of Books,
28 Little Russell Street
London, WC1A 2HN
letters@lrb.co.uk
Please include name, address, and a telephone number.